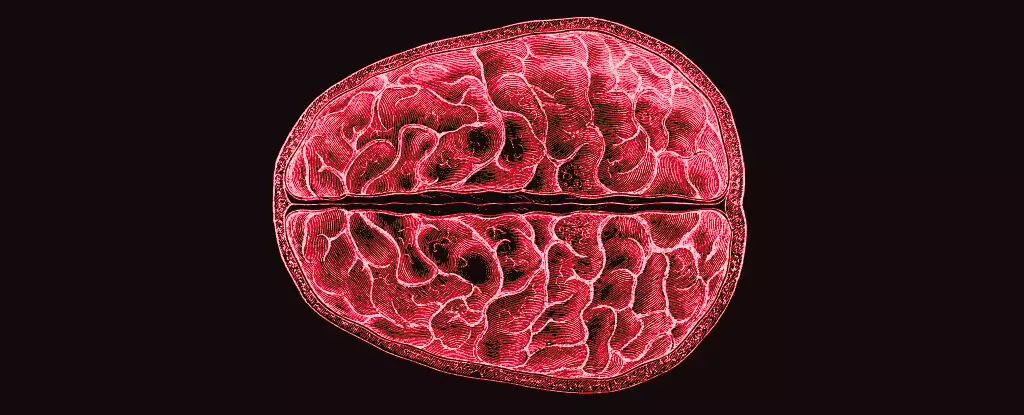
The fascinating interplay between hormones and brain structure is an area that has long been overshadowed by more visible aspects of the menstrual cycle. Most discussions about menstruation revolve around the obvious physical changes and emotional responses women experience. Yet, groundbreaking research from a team led by neuroscientists Elizabeth Rizor and Viktoriya Babenko at the University of California, Santa Barbara, sets the stage for a paradigm shift in the understanding of how the menstrual cycle deeply influences brain architecture. This pioneering study uncovers the intricate ways in which hormonal fluctuations may alter not just the reproductive organs, but the very neural networks within women’s brains.
Research Findings: A New Era in Understanding
Published in a peer-reviewed journal in 2023, the team meticulously documented brain changes across the menstrual cycle in 30 women. Their work marks the first time that simultaneous changes across the brain’s white matter microstructure and cortical thickness have been analyzed in relation to hormonal changes induced by the menstrual cycle. This isn’t merely an academic curiosity; it provides vital clues linking hormonal variations to potential cognitive and emotional outcomes in women.
Rizor and Babenko’s findings resonate profoundly, suggesting that the effects of hormones extend beyond traditional areas of focus. “Strong brain-hormone interaction effects may not be limited to classically known hypothalamic-pituitary-gonadal-axis (HPG-axis) receptor-dense regions,” the study authors state confidently. This challenges long-held beliefs and calls for a more nuanced exploration of how menstruation influences the entire brain, rather than just localized regions associated with reproductive functions.
Empirical Evidence: MRI Insights
To unveil the brain’s response to hormonal changes, the researchers employed MRI scans during three pivotal phases of the menstrual cycle: menses, ovulation, and mid-luteal. Each of these phases brought unique hormonal profiles, which were precisely tracked and analyzed. The research indicated that as estrogen and other hormones fluctuate, structural changes in the brain unfold, including shifts in gray and white matter volume and changes in cerebrospinal fluid levels.
One particularly striking observation arose during the pre-ovulatory phase when levels of 17β-estradiol and luteinizing hormone surged. MRI data revealed that these hormonal peaks were linked to enhanced white matter alterations, suggesting an increase in the speed of information transfer between different brain regions. This could hint at heightened cognitive abilities or emotional responses during this critical time, although the implications of these changes require further investigation.
Interestingly, the hormone fluctuations are not just constrained to cognitive enhancements. For instance, the rise of follicle-stimulating hormone was associated with a thickening of gray matter, potentially indicating an expansion in neural connectivity. After ovulation, as progesterone levels increased, fluctuations in tissue volume and decreased cerebrospinal fluid were observed — changes which could have profound implications for mood and cognitive function during the luteal phase.
Addressing the Research Gap: The Menstruation Dilemma
Despite the significance of these findings, one cannot help but question why menstrual-related research has remained limited for so long. It’s a mystery that lingers in an era of scientific advancement, particularly considering that half the world’s population experiences menstruation. The societal stigmas surrounding these natural processes have likely stunted scientific inquiry and public discourse, relegating menstruation to a topic that is often considered taboo.
The result is an alarming knowledge gap regarding the physiological and psychological effects of the menstrual cycle. Rizor, Babenko, and their colleagues note that while the cyclic hormonal fluctuations have substantial behavioral and structural impacts on the central nervous system, the specific mechanisms are still murky. Their research endeavors to illuminate these paths, marking the beginning of a much-needed conversation about women’s health that encompasses neurological aspects previously ignored.
The Future of Women’s Health Research
What these findings imply is not just a scientific curiosity but a call to action for future research. The implications for understanding mental health disparities that are often exacerbated by hormonal changes cannot be understated. Unraveling these complexities may lead to better-targeted therapies for period-related mood disorders, anxiety, and depression. As we stand on the precipice of a new understanding of how menstrual cycles affect the brain, the need for comprehensive studies cannot be overstated.
The revelations from this research offer a hopeful glimpse into a future where female health is fully understood in all its dimensions, integrating hormonal cycles with brain function — a paradigm that could change how society responds to women’s health issues on a global scale.